NDE DISCLOSURE DISCRIMINATION
Those who have a near-death experience (NDE) struggle with sharing this information with their healthcare providers, family members, and others. Some struggle to make sense of the experience, mainly if they are unaware that others have reported similar accounts. Though it’s challenging to explain NDEs scientifically, they happen to millions of people and often leave individuals profoundly changed for the remainder of their lives. Studies have found that 10 – 20% of people who are resuscitated after nearly dying have an NDE: an out-of-body experience accompanied by various perceptions such as traveling through a tunnel of light, feeling loved, and/or being received by deceased loved ones. Most NDEs are highly pleasurable experiences, but a percentage describe a distressing experience, which can be traumatizing to patients.
HEALTHCARE PROVIDER EDUCATION
Most healthcare providers receive no training on how to respond to a patient’s report of an NDE. Yet, how they treat patients following these experiences can have long-term impacts. Patients who tell a healthcare worker about their experience sometimes end up feeling ignored, having their experience disregarded as non-factual, or being misdiagnosed with hallucinations or a mental disorder. This is referred to as a “gap in medical care for near-death experiencers” because it can unwittingly harm the individual and cause patients to avoid future discussion of their experience out of fear that they will be stigmatized.
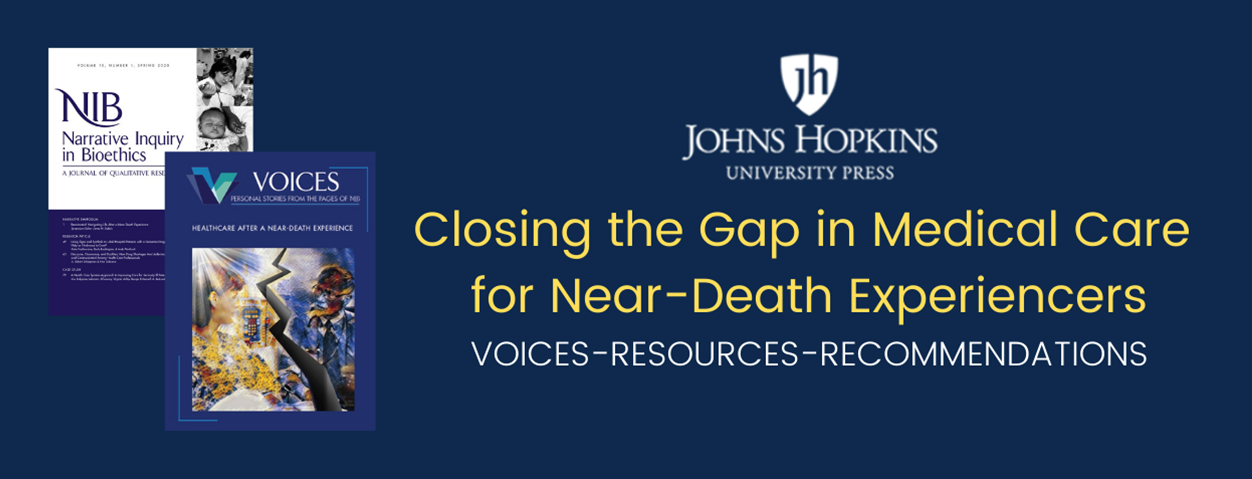
ABOUT THE VOICES ISSUE
In the winter of 2020, Narrative Inquiry in Bioethics: A Journal of Qualitative Research (NIB; Vol. 10, No. 3) published a special issue on “Healthcare After a Near-Death Experience.” The issue contained a collection of personal stories from individuals who had an NDE as well as articles by healthcare and other professionals. IANDS raised money to have this material published in VOICES: Personal Stories from the Pages of NIB, produced for the Foundation for Narrative Inquiry in Bioethics by Johns Hopkins University Press. This issue of VOICES contains the articles from the NIB issue, including 18 near-death experiencers who share what happened and how they felt about disclosing their NDE to healthcare providers and family. The hope is that these accounts will serve as an educational resource to help patients, families, and healthcare providers to close the gap of care for experiencers.
RESOURCES FOR
Closing the Gap in Medical Care for Near-Death Experiencers
Video and audio resources
Medical Training Video
This groundbreaking video features six highly qualified medical professionals, including Dr. Eben Alexander, best-selling author of Proof of Heaven, and Dr. Bruce Greyson, pioneering and currently foremost NDE researcher. In addition, near-death experiencers describe their amazing journeys into the afterlife and back. Originally created to prepare medical health, mental health, and spiritual/religious health professionals to respond to NDE disclosure with ethical best practices, this video captivates general audiences, as well.
Near-Death Experience,
What Medical Professionals Need to Know
Note: Turning on subtitles/closed captions is recommended.
Also, a media review of this video can be found here.
Also, a media review of this video can be found here.
Veterans’ NDE Video
Veterans who have had near-death experiences (NDEs) may experience a gap in healthcare. Most healthcare providers have little training to recognize NDEs and frequently confuse them with post-traumatic stress (PTS) or mental illness. Therefore, veteran NDErs may be ignored, misdiagnosed, over-medicated, and given costly, ineffective treatment. Hear veterans, their family members, counselors, and researchers share their insights into these powerful transcendent experiences and the need for appropriate responses by healthcare providers.
A Gap in Care for Veterans Who Have Had NDEs
Note: Turning on subtitles/close caption is recommended.
Healthcare Professionals' Training Video
In this video, Dr. Jan Holden from the University of North Texas interviews a near-death experiencer, Leslie, about her distressing experience disclosing her NDE to medical professionals. Jan then presents results of a study indicating how frequently NDErs have felt harmed by disclosing their NDEs to medical health, mental health, and spiritual/religious health professionals, as well as family and friends. She concludes with recommendations for healthcare professionals and others to incorporate into their response to NDE disclosure—recommendations that enable the health professional to uphold their ethical mandate (and family and friends to uphold their personal moral code) to do no harm to near-death and related experiencers.
Healthcare Professionals' Response to NDE Disclosure
• Also see https://www.janholden.com/videos
• Reference: Holden, J. M., Kinsey, L., & Moore, T. R. (2014). Disclosing near-death experiences to professional healthcare providers and non-professionals. Spirituality in Clinical Practice, 1(4), 278–287.
2021 IANDS Spring Symposium: Providing Healthcare to Near-Death and Related Experiencers

Other Publications
Responding to Near-Death and Related Experiences:
The purpose of this one-day online symposium was for anyone—professional or layperson—to complete the day feeling confident that they know how to fulfill their professional ethical and personal moral responsibility to do no harm to near-death and related experiencers. Contributors included healthcare providers (medical, mental, social, and spiritual), a bioethicist, family members and friends, as well as experiencers themselves who revealed their best and worst experiences of disclosure and offered their most important advice about how others can avoid harm and increase help to those touched by near-death and related experiences. Through April, 2023, nurses can earn continuing education credit by viewing the Symposium recording. The recording can be purchased and accessed here.

The Day I Died Documentary
The 2006 BBC documentary The Day I Died, available at no cost online, is still relevant today, featuring leading researchers in the field of near-death studies addressing the ways in which NDEs challenge the materialist worldview that currently dominates Western scientific inquiry. Teachers can use the viewing/teaching guide. A 2006 media review of the video can be found here. A study showing the effectiveness of using The Day I Died as an educational tool can be found here.
Physician Reports a Case of Veridical Perception
In this video, Dr. Lloyd Rudy reports a case of veridical perception—perception during an NDE that is later verified as accurate—in which Dr. Rudy was the attending physician. The evidential nature of the veridical perception is particularly strong in that what the patient “saw” during his NDE was idiosyncratic and could not have been deduced through hearing.
IANDS website resources
Other Publications
An overview of the status of education about NDEs as of 2009:
Foster, R., James, D., & Holden, J. M. (2009). Practical applications of near-death experiences research. In J. M. Holden, B. Greyson, & D. James (Eds.), The handbook of near-death experiences: Thirty years of investigation (pp. 235–258). Praeger/ABC-CLIO.
A report of a study about the effectiveness of an online educational program on NDEs for licensed counselors:
Loseu, S., & Holden, J. M. (2017). Impact of an online education program on counselors’ knowledge and attitudes about near-death experiences. Journal of Near-Death Studies, 36(1), 3–26.
A report of a study about the effectiveness of an educational program on NDEs for undergraduates:
Tassell-Matamua, N., & Lindsay, N. (2017). Undergraduate psychology students' knowledge and attitudes about near-death experiences: Does education about NDEs make a difference? Journal of Near-Death Studies, 36(1), 27–52.
A report of a study about physician trainees’ metaphysical experiences and their relationship to end-of-life care:
Schmit, J. M., & Meyer, L. E. (2020). Metaphysical beliefs and experiences among physician trainees: An exploratory study. Journal of Near-Death Studies, 38(3), 137–156.
A casebook of veridical NDEs -- experiencers' perceptions during NDE later verified as accurate:
Rivas, T., Dirven, A., & Smit, R. H. (2023). The Self Does Not Die: Verified paranormal phenomena from near-death experiences (2nd ed.). IANDS Publications.
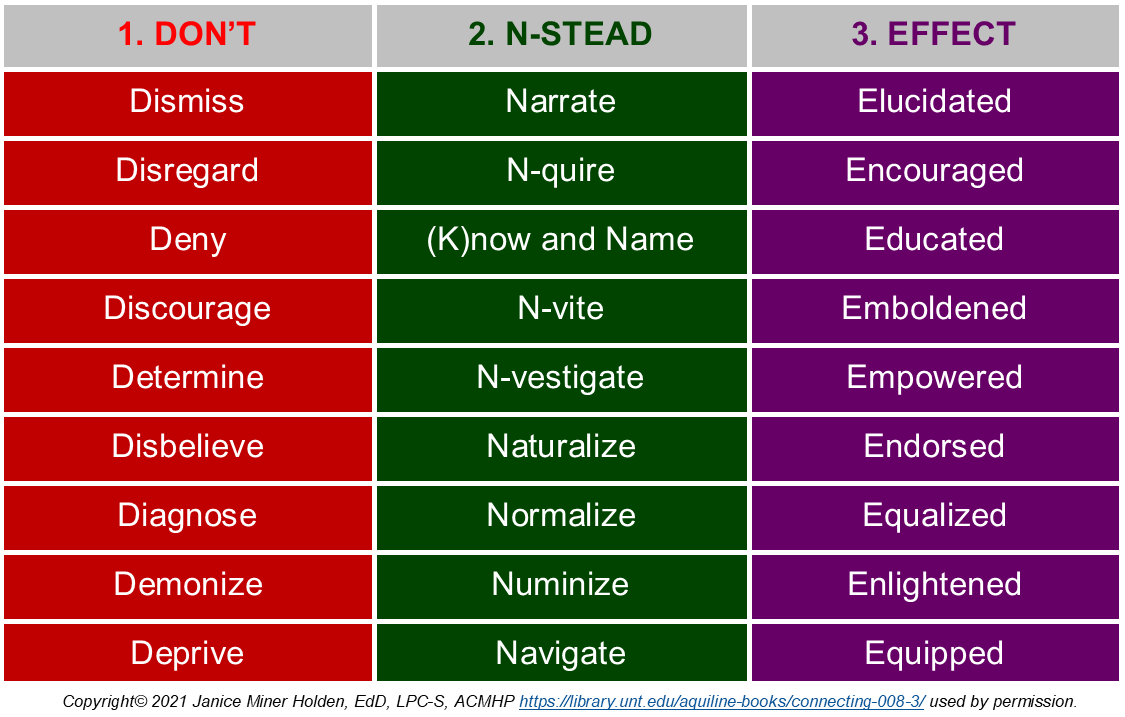
Responding to Near-Death and Related Experiences:
Recommendations for Healthcare Providers
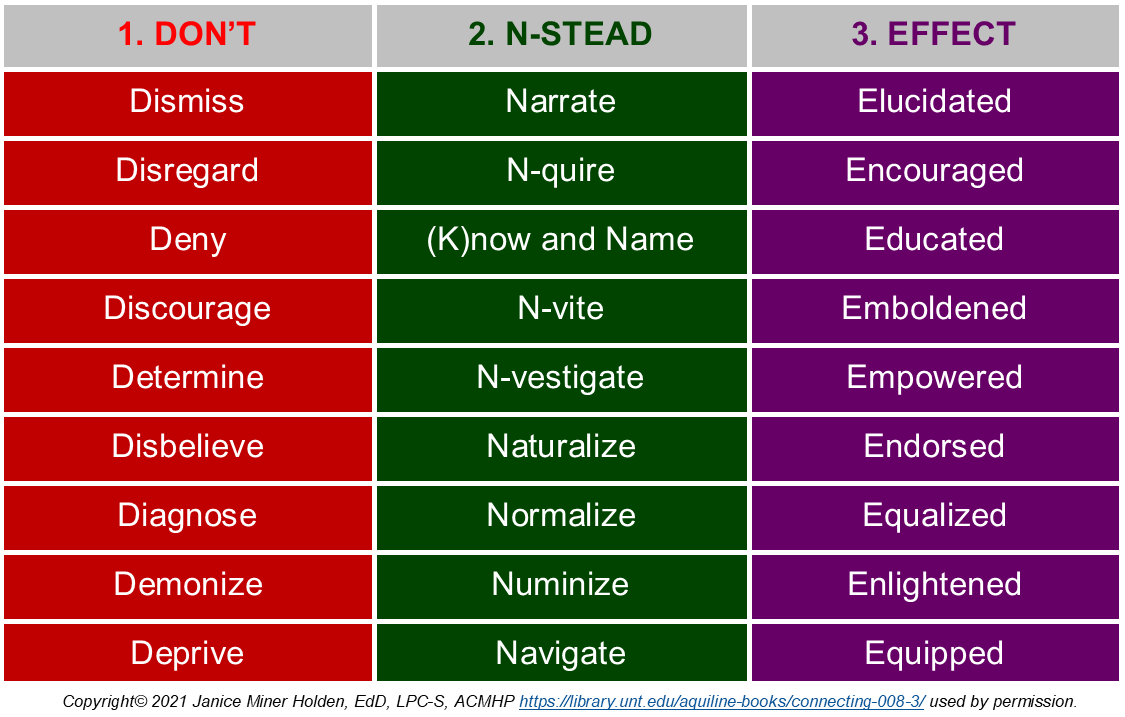
1. Don’t:
- Dismiss the possibility that the person in distress is experiencing an NDE or related experience.
- (In case of possible NDE or related experience) Disregard the possibility that an experience may have occurred.
- (In case of disclosure of NDE or related experience) Deny the experience as one that has been professionally recognized and labeled.
- Discourage the experiencer from talking about it and/or psychospiritually processing its aftereffects and meaning.
- Determine the meaning of the experience for the experiencer.
- Disbelieve that the experience was—or, at least, could be—real.
- Diagnose the experience or experiencer as a sign of mental illness, based on the experience alone.
- Demonize the experience, by default, as spiritually malevolent or evil.
- Deprive the experiencer of resources for further information and support.
2. N-stead:
-
(In case of search-and-rescue or resuscitation) Narrate your activities and intentions, either out loud or silently.
- (In case of possible NDE or related experience) N-quire (inquire) whether client remembers anything noteworthy or unusual from the time during their medical crisis or other extreme circumstances.
- (In case of disclosure of NDE or related experiences) (K)now and name the experience as it is referred to in the professional literature—while being open to a preferred term that the experiencer may have.
- N-vite (invite) the experiencer to talk about the experience, its aftereffects, and its meaning.
- N-vestigate (investigate) the meaning the experiencer attributes to the experience.
- Naturalize the experience as real or potentially real.
- Normalize the experience as common and not inherently related to mental illness.
- Numinize the experience as spiritually neutral, benevolent, or potentially benevolent—except in case of explicit malevolent content.
- Navigate the experiencer to resources for further information and support.
3. Effect of the N’s is that the experiencer likely will feel:
- Elucidated regarding your actions and intentions.
- Encouraged to disclose whatever experiencer wishes to.
- Educated that the experience is a known phenomenon with a name.
- Emboldened to discuss the experience, its aftereffects, and its meaning as much as the experiencer wishes.
- Empowered to reflect on and generate one’s own meaning.
- Endorsed as having had a legitimate and real or potentially real experience.
- Equalized that the experience itself does not render the experiencer “crazy.”
- Enlightened that the experience likely was not inherently “evil” and is potentially spiritually beneficial.
- Equipped to find further information and support.
Responding to Near-Death and Related Experiences:
Recommendations for Healthcare Providers